Featured Scientist: Aaron Brown (he/him/his), PhD and Licensed Clinical Social Worker (LCSW), Assistant Professor at University of Kentucky with the College of Social Work.

Birthplace: Cleveland, Tennessee
My Research: My research interests include rural social work, treatments for addiction, and harm reduction. A lot of my work has been focused on creating and using text messages as interventions. The goal of this approach is to reduce harm for people who are struggling with substance use disorders.
Research Goals: I want to find ways to improve treatment for people with opioid use disorder. This includes the use of medications. I am particularly interested in the use of extended-release naltrexone. I also want to increase access to harm reduction in Appalachian communities.
Career Goals: I hope to develop a research program that can make a positive impact on the field of social work.
Hobbies: I love spending time outdoors including kayaking and hiking. I also enjoy playing video games and watching TV.
Favorite Thing About Science: I love how science incorporates a lot of different tasks and requires many skills. It never gets boring.
Scientist Upbringing: I have always enjoyed reading and writing. And I have always loved science. It took me a long time to get to my current career as a social scientist and social work scholar. I am actually grateful for that. My past experiences as a social worker and clinician gave me a passion for the topics I research. I practiced as a social worker in rural Appalachian communities that were ravaged by the opioid crisis. I saw that those communities needed better access to evidence-based interventions. It motivated me to pursue a career in research. I also learned that I really enjoy statistics and intervention research.
My Team: I work on a few different teams. I work with two colleagues who I went to school with at the University of Tennessee: Aubrey Jones and Jayme Walters. I enjoy working with them so much. We take turns leading different projects and papers. We work really well together. I often contribute with methods and analysis, as well as helping to write and edit papers. I have also worked on a large team at the Center for Behavioral Health and Research at the University of Tennessee, where I have helped implement interventions for clinical trials. My role on that team has been as an implementation specialist. I have contributed to automation and the various technologies we use for our studies. I have also served as a clinical consultant on projects.
Organism of Study: I have several research areas. My primary interest is on treatments for opioid use disorder.
Field of Study: Social Work and Addictions
What is Social Work and Addictions? I study treatments for addiction. These treatments include those based on therapy and those based on medication. As a social worker, I’m interested in how we can create effective interventions that help address addiction.
Check Out My Original Paper: “Health professionals’ attitudes toward medications for opioid use disorder” published in Substance Abuse.

Citation: Brown, A. R. (2021). Health professionals’ attitudes toward medications for opioid use disorder. Substance Abuse, 43(1), 598–614.
Article written by undergraduate students enrolled in the social work program at Utah State University, with support from Dr. Mercedes Castro Cabado, a researcher working at AkzoNobel in North Rhine-Westphalia, Germany.
Research At A Glance: The opioid crisis is harming many people in the U.S. While Americans make up less than 5% of the world’s population, they consume over 99% of the world’s hydrocodone and 80% of the world’s oxycodone. Research shows that some medications can be used to help people impacted by opioid use disorder (OUD). OUD is a chronic brain disease caused by the continued use of opioids. An opioid is a chemical substance often prescribed by doctors to help to reduce pain. A person impacted by OUD often feels the need to keep using opioids on a regular basis, even if the pain goes away. They can become very sick and struggle with day-to-day activities. Medications for opioid use disorder (MOUDs) can reduce death rates and prevent relapse. Some common MOUDs include buprenorphine, methadone, and naltrexone. These medications can help to reduce cravings and prevent withdrawal symptoms. The authors of this article present a review to summarize our understanding of the attitudes that health professionals have about MOUDs. The authors found that the attitudes that health professionals have about MOUDs affect their decisions to prescribe them. As a result, these attitudes also affect access for patients. When a health professional believes that abstinence is the best way to treat OUD, they are less likely to prescribe MOUDs. When health professionals argue for abstinence, they expect people to avoid the use of all drugs, including MOUDs. The authors found three factors associated with more positive attitudes toward MOUDS and the increased use of MOUDs: exposure, training, and knowledge. When prescribing professionals work with pharmacists, MOUDs become more accessible. This creates an open dialogue between different types of health professionals working with people struggling with OUD.
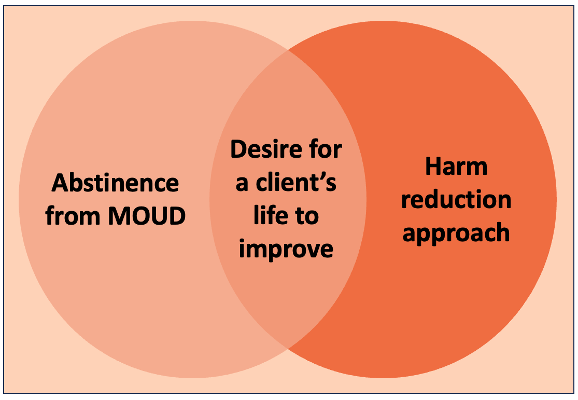
Highlights: The authors found that health professionals tend to have two main approaches to treating people with OUD: abstinence or harm reduction (Figure 1). Harm reduction focuses on empowering people affected by OUD to make a positive change in their lives. This happens by providing them with life-saving tools and information to make their own choices. MOUDs are some of the tools offered to treat OUD for those who take a harm reduction approach. The authors found that medical professionals are more likely to support the use of MOUDs than other health professionals. Training, knowledge, education, tenure, and exposure are all important factors that lead to the increased use of MOUDs. For example, the authors found that physicians tend to take an abstinence approach if they lack the support of addiction specialists. They are more likely to take an abstinence approach because they have limited experience with MOUDs. However, they are more willing to follow the harm reduction approach when they are trained in the use of MOUDs and have interactions with patients who are receiving MOUD treatment.
What My Science Looks Like: In this review, the authors found previously published research articles about attitudes and beliefs toward MOUDs. The authors carefully chose articles that would be included in the study. They used specific criteria to select articles that were the most relevant to their research question. The peer-reviewed articles were found in educational databases and were conducted between 1997-2021. The articles had to be original research that looked at health professionals in the U.S. or second-hand studies that also included U.S. health professionals. The articles also had to focus on attitudes that health professions have about MOUDs. Using this process, the authors found that when providers know more about MOUDs, have more acceptance towards MOUDs, and more awareness about addiction, they are also more willing to prescribe them (Figure 2).

The Big Picture: Opioid misuse and the OUD crisis in the U.S. is costly to families and communities. According to the Centers for Disease Control (CDC), 44 people die every day from overdoses involving prescription opioids. However, solving the OUD crisis is complex. Medications could be a driving force in decreasing opioid misuse in the U.S. MOUDs can reduce the loss of life and prevent relapse for those with OUD. Attitudes about the effectiveness of MOUDs are associated with their use and accessibility. Exposure to MOUDs through practice and training can allow health professionals to learn more and can lead to more positive attitudes about MOUDs use.
Decoding The Language:
Abstinence: Abstinence is the practice of restraining oneself from using drugs or drinking alcohol.
Extended-release naltrexone: Extended-release naltrexone isa way to administer naltrexone to patients. The naltrexone is injected by a health professional with a syringe once a month. Naltrexone is one of the common medications used to treat OUD.
Harm reduction: Harm reduction refers to treatments that are designed to reduce the negative consequences associated with drug use. Harm reduction can be considered an alternative to abstinence.
Medications for Opioid Use Disorder (MOUD): MOUDs are drugs that bind to the parts of the brain that give people pleasurable feelings. These are the same parts of the brain that opioids bind to. The difference is that MOUDs do not produce the same “high” as opioids and they are used as a treatment for addiction. Common MOUDS Include Methadone, Naltrexone, and Buprenorphine.
Opioid: An opioid isa drug that causes the brain to release large amounts of dopamine, which causes pleasurable feelings that can be described as a “high”. Opioids can also have many negative side effects such as confusion, nausea, and brain damage. Examples of common opioids include heroin, synthetic opioids such as fentanyl, and pain relievers available legally by prescription, such as oxycodone, hydrocodone, codeine, morphine.
Opioid crisis: The opioid crisis refers to the ongoing misuse of opiate drugs in the U.S., which has led to a declining health and death.
Opioid Use Disorder (OUD): OUD is an illness that a person can develop when misusing opioids such as morphine, fentanyl, and codeine. Consistent misuse of opioids can lead to an overpowering desire to use opioids and to increase the amount of opioids that are used. People who struggle with OUD often experience withdrawal symptoms when they stop. These can include general pain, diarrhea, fever, dilated pupils, agitation, anxiety, nausea and vomiting, intense cravings, elevated heart rate and blood pressure, sweating and insomnia.
Relapse: Relapse takes place when someone who has struggled with addiction has stopped using drugs or alcohol but begins to use them again.
Substance use disorder: Substance use disorder is a treatable mental condition that affects a person’s brain and behavior. It is characterized by the inability to control the use of legal or illegal drugs, alcohol, or medications.
Learn More:
A Daily Podcast episode from the New York Time on the way OUD is being treated at a harm reduction clinic in Vancouver, Canada.
A YouTube video about the epidemic and how opioids work and become addictive.
A research article on the decrease in opioid-therapy prescribing rates in a family medicine practice, which offer chiropractic services:
Rosa, J., & Burke, J. R. (2021). Changes in opioid therapy use by an interprofessional primary care team: A descriptive study of opioid prescription data. Journal of Manipulative and Physiological Therapeutics, 44(3), 186-195.
A research article on the relation between the driving time to the therapy center and the completion rate of the treatment with methadone:
Alibrahim, A., Marsh, J. C., Amaro, H., Kong, Y., Khachikian, T., & Guerrero, E. (2022). Disparities in expected driving time to opioid treatment and treatment completion: Findings from an exploratory study. BMC Health Services Research, 22(1).
A research article on availability of facilities across United States, offering both, services focusing on LGBTQ+ population and OUD treatment: Paschen-Wolff, M. M., Velasquez, R., Aydinoglo, N., & Campbell, A. N. C. (2022). Simulating the experience of searching for LGBTQ-specific opioid use disorder treatment in the united states. Journal of Substance Abuse Treatment, 140.
Synopsis edited by Dr. Rosario Marroquín-Flores, Texas Tech University, Department Biological Sciences and Dr. Jayme Walters, Utah State University, Department of Social Work.
Download this article here
Please take a survey to share your thoughts about the article!